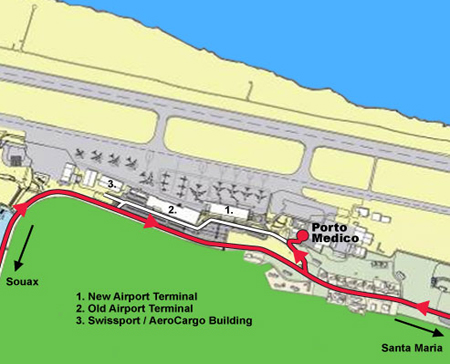
Medical Services & Travel Clinic
Hato International Airport, Curaçao, Dutch Caribbean
Tel: (+5999) 888 7511
E-mail: info@portomedico.com

Porto Medico is located at the Curaçao International Airport, between Curoil and Catering KLM building.
Disease Prevention
Covid-19
To stay informed about the current global pandemic, Covid-19, otherwise known as the Corona virus, we strongly advise you to visit the following websites. You will be able to find updates, information and advice on how to best protect yourself and those around you from the virus.
WHO Covid - 19:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019
CDC Covid-19
https://wwwnc.cdc.gov/travel
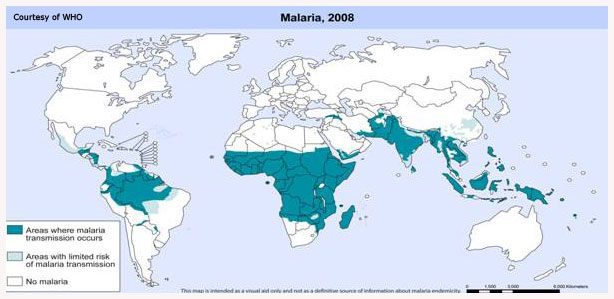
Malaria
Malaria is a common and life-threatening disease in many tropical and subtropical countries. It is an acute febrile illness transmitted by Anopheles mosquito's, which bite mainly between sunset and sunrise. There is no vaccination available, so prevention consists of a combination of preventive medication (profylaxis) of anti-malaria tablets and avoidance of mosquito bites (e.g. use of bednet and insect repellent). Avoiding mosquito bites remains the cornerstone of protection against malaria.DO NOT GET BITTEN!
- Avoid bites at all times in all malaria risk areas.
- Cover up with long sleeves, trousers, socks and shoes (90% of mosquito bites occur below the knees!).
- Apply DEET (diethylmetatoluamide) insect repellent to exposed skin.
- Only sleep in air-conditioned or screened accommodation or carry an insecticide-impregnated bed net - and sleep under it!
Malaria transmission is rare in areas above 2000 meters.
Travelers should seek advice on the risk of malaria in specific areas and time of year.
The recommended prophylaxis for each country is decided on:- the risk of contracting malaria
- prevailing species of malaria parasites in the area
There are 5 species of Malaria: Plasmodium Falciparum, Pl. Vivax, Pl. Ovale, Pl. Malariae,
Pl. Knowlesi - level and spread of drug resistance reported from the area
- possible side effects of the tablets.
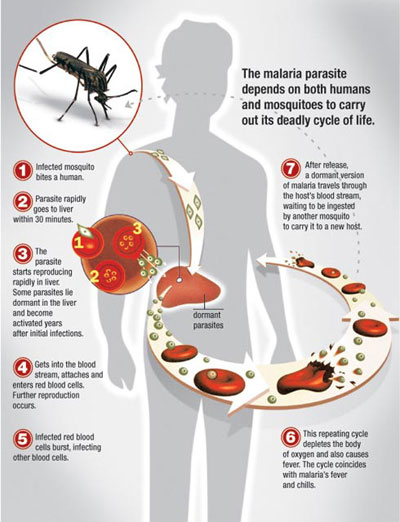
Malaria chemoprophylaxis kill the malaria parasite before the traveler becomes clinically ill. They act mostly on the parasites in the blood phase, either immediately after an infected bite, or when the parasites exit the liver at the end of the ‘incubation period’.
Chemoprophylaxis must therefore be commenced before entering the malaria area, to ensure that protective drug levels are reached and that the drugs are tolerated. Likewise prophylaxis have to be continued for 4 weeks after leaving the area to ensure eradication of parasites still emerging from the liver. Only the malaria profylaxe Malarone®, which acts on the liver stage of the parasites, can be stopped seven days after leaving the malaria area.
No drug or bite prevention method is 100% effective, but chosen and applied well, the combination can provide 90% protection against malaria illness and death. It has been shown that even if illness does occur, the likelihood of cerebral malaria is diminished and the chance of death reduced significantly.
No drug is completely without side effects. The decision whether to use preventive drugs or not should be based on the relative malaria risk in the area to be visited, any pre-existing disease or chronic medication the traveler may have or use, the potential side effects and cost of the available appropriate anti-malaria drugs.
Both personal protection methods and anti-malaria medications are important, and neither should be neglected at the expense of the other !
Seek early treatment; Any flu-like illness (fever, headaches, shivers, muscle aches, vomiting and even diarrhea) beginning after 7 days and for up to 3 months or even longer after leaving a malaria risk region, should be presumed to be malaria ! This is regardless of whether you think you have been bitten and /or malaria prevention tablets have been taken correctly or not. Make sure that the diagnosis is confirmed by a reliable laboratory.
Links:CDC - Malaria
WHO - Malaria
Traveldoctor - Malaria
Dengue


There is a high incidence of Dengue in the Caribbean and other (sub-)tropical areas.
Transmission occurs from the bite of an infected Aedes aegypti (rarely Aedes albopictus) mosquito. Mosquitoes first become infected with dengue virus by feeding on the blood of a dengue-infected person. After the virus replicates for 8–12 days in the mosquito, the mosquito can transmit dengue virus to many other people. It cannot be spread directly from human to human.
The risk of being bitten is highest during the early morning, several hours after daybreak, and in the late afternoon several hours before sunset, because the female mosquito typically feeds (bites) during these hours. However, mosquitoes may feed at any time during the day

The Dengue viruses encompass four different serotypes, each of which can lead to Dengue Fever and Dengue Haemorrhagic Fever.
Incubation period ranges from 3 to 14 days, commonly 4 to 7 days.
Symptoms
Dengue Fever is clinically characterized by sudden onset of high fever, severe headache, pain behind the eyes, muscle and joint pains, loss of appetite, nausea and rash. Young children may exhibit a milder non- specific febrile illness with rash.
Dengue Haemorrhagic Fever is a severe and potentially fatal complication of Dengue Fever. Initially, the features include high fever, which last two to seven days and can be as high as 40-41º C, facial flush and other non constitutional symptoms of Dengue Fever. Later, it may be followed by the manifestation of bleeding tendency, such as skin bruises, nose or gum bleeding and possible internal bleeding. In severe cases, it may progress to circulatory failure, shock and death.
Diagnosis is usually confirmed by serologic tests. Because specific antibodies (IgM) take several days to develop (usually present by day 5 of the illness) early testing is not recommended.
Immunity is gained against that serotype after recovery from its infection. However, no effective protection is conferred against subsequent infection by the other three serotypes.
Treatment
There is no specific medication for Dengue Fever or Dengue Haemorrhagic Fever. Dengue Fever is mostly self-limiting. Symptomatic treatment is given to provide relief from fever and pain. Paracetamol or Acetaminophen is recommended.
Avoid non-steroidal anti inflammatory agents like Ibuprofen, Diclofenac, Naproxen, Aspirine etc. Patients with Dengue Haemorrhagic Fever should be treated promptly with supportive management. The mainstay of treatment is to maintain the circulating fluid volume. With appropriate and timely treatment, mortality rate should be less than 1%.
Preventive Measures for Travelers
- Neither vaccine nor drugs for preventing Dengue infection do exist.
- Travelers should be advised to take measures to avoid being bitten by Aedes mosquitoes.
- Select accommodations with well-screened windows or air-conditioning when possible. Aedes mosquitoes typically live indoors and are often found in dark, cool places such as in closets, under beds, behind curtains, and in bathrooms. A traveler should be advised to use insecticides to get rid of mosquitoes in these areas.
- Wear light colored clothing adequately covers the arms and legs, especially during the early morning and late afternoon.
- Apply insect repellent to both skin and clothing (e.g., permethrin). The most effective repellents contain DEET (N,N-diethylmetatoluamide).
- Empty and clean or cover any standing water that can be mosquito-breeding sites in your accommodation (e.g., water storage barrels).
Link: CDC - Dengue
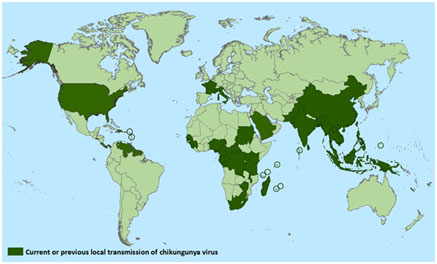
Chikungunya

Chikungunya is a viral infection transmitted by mosquitoes (Aedus aegypti and Aedes albictus) to people. These mosquitoes bite during daytime.
These mosquitoes also transmit the Dengue virus.
The Chikungunya infection was first identified in October 2013 in the Americas and outbreaks have since then also occurred in the Caribbean.
The incubation time is from 2 up to 12 days. Not all individuals infected with the virus will develop symptoms.
Symptoms of Chikungunya infection:
- Acute onset of fever
- Joint aches, which usually occur symmetrically in the hands and feet. This can be very severe and disabling.
- Headaches
- Fatigue
- Nausea
- rash on limbs and trunks
- muscle aches
- stiffness of the joints or swollen joints of hands and feet.
Recovery time:
Most people who get sick feel better within 3 to 10 days. For elderly it might take a few months. In extreme cases one might suffer from joint aches and stiffness for up to 3 years.
Chikungunya disease rarely results in death.
It is believed that once exposed to the Chikungunya virus, individuals will develop long lasting immunity that will protect them against a new infection.
Diagnosis of Chikungunya infection is by blood testing:
- Low count of white blood cells and platelets, and elevated liver tests (transaminases) are the most common clinical laboratory findings. Confirmation is by:
- Viral culture to detect virus in first 3 days of illness
- RT-PCR to detect viral RNA in first 8 days of illness
- Serology to detect IgM, IgG, and neutralizing antibodies that develop toward the end of the first week of illness (≥4 days after illness onset)
There is no specific treatment or vaccine for the Chikungunya infection.
To relieve symptoms Paracetamol is recommended.
If Dengue has been ruled out, non-steroidal anti-inflammatory drugs like Diclofenac, Ibuprofen, Celebrex etc. may be used to relieve the joint aches and stiffness.
"Do not get bitten"

- Wear light colored, long sleeved shirts and long trousers
- Apply Deet to exposed skin and /or clothing. Deet remains the golden standard of presently available insect repellents. Avoid Deet in mouth and eyes. Beware of plastics and rubber, which may be affected by Deet.
- Use Permethrim impregnated bed nets. Permethrin is a contact insecticide, causing nervous system toxicity, leading to death or "knock down" of the insect. It is said that the room with impregnated mosquito nets have 70 % less mosquitoes in the room.
- Select accommodations with well-screened windows or air-conditioning when possible. Aedes mosquitoes typically live indoors and are often found in dark, cool places such as in closets, under beds, behind curtains, and in bathrooms. One should be advised to use insecticides to get rid of mosquitoes in these areas. Empty and clean or cover any standing water that can be mosquito-breeding sites in your accommodation (e.g., water storage barrels).
 Distribution of Chikungunya in the Caribbean (july 29, 2014)
Distribution of Chikungunya in the Caribbean (july 29, 2014)
Link: CDC - Chikungunya
Zika

Zika is a virus infection transmitted by mosquitoes (Aedus Aegypti and Aedus Albictus) to people.
These mosquitoes bite during day time and also transmit Dengue fever, Chikungunya, Yellow fever and West Nile fever.
Zika fever occurs about 2 to 7 days after the mosquito bite.
Although the disease is very mild, the effects to the infected unborn child and also neurological complications are causing a lot of fear of this new virus.
During the first week of infection, Zika virus can be found in the blood and passed from an infected person to another mosquito through mosquito bites. An infected mosquito can then spread the virus to other people. Also sexual transmission has been reported.
Symptoms of Zika
Usually mild and can last 2 to 7 days. The most common symptoms are:- Slight fever
- Headaches
- Joint aches / body aches
- Skin rash
- Conjunctivitis (red eye irritations)
- General malaise
One out of 5 people infected with the virus will become ill. For this reason many people do not realize they have been infected with this virus.
Zika and pregnancy, The virus can be transmitted from a pregnant woman to her baby during pregnancy and during time of birth, causing a high number of infant deaths and high number of cases of babies with microcephaly, a rare condition in which the infants are born with shrunken skulls. Breastfeeding seems to be safe.
Neurological complications, the disease can lead to serious neurological complaints, including meningitis and M. Guillain Barre (affecting the nervous system).
Laboratory diagnosis, is by blood and urine tests (RT-PCR)
Treatment:
- No vaccine or medications are available to prevent or treat Zika infections.
To relieve fever and pain take Paracetamol. If Dengue fever has been ruled out non- steroidal anti-inflammatory drugs like Diclofenac, Ibuprofen may be used to relieve the fever and body aches.
Prevention:
One is advised to take measures to avoid being bitten by the Aedus mosquito; the same prevention as against Dengue fever and Chikungunya.
Yellow Fever


Yellow fever is a type of virus known as a flavivirus. The virus is transmitted through mosquito (Aedes Aegypti) bites. It can be spread from one host to another, usually between monkeys, or from monkeys to humans, or from person to person. The mosquitoes live and breed in jungle and urban areas in tropical Africa and South America. The mosquito bites during the daylight hours.
The virus causes sudden onset of fever, four days after the bite. Most cases are mild, last less than a week, and the person makes a full recovery. Sometimes it is more serious. The liver may be damaged leading to jaundice - a yellowish tinge to the skin. Hence the name 'yellow' fever. It may cause joint pain and vomiting. Eventually the clotting system fails and bleeding occurs from the nose, gums, stomach and skin. Up to ten percent of sufferers will die 7 to 10 days after the onset of the illness.
There is no treatment for the disease "yellow fever".
Travelers immunized against yellow fever are issued with an internationally recognized vaccination certificate for inspection by immigration officials. The international health regulations concerning yellow fever are unequivocal, and unvaccinated travelers may face denial of entry, or even quarantine in certain circumstances.This strict control of yellow fever vaccinations is maintained to:
- protect individual travelers who may be exposed to yellow fever infection. As yellow fever is frequently fatal, vaccination is recommended for all travelers visiting areas where the risk of exposure is high.
- protect countries from the risk of importing yellow fever virus. This is mandatory vaccination and required for entry of countries or areas concerned.
Porto Medico is a designated "Yellow Fever Vaccination Center".
Link: CDC - Yellow Fever
Hepatitis A
Hepatitis A is an acute contagious liver disease caused by the Hepatitis A virus, lasting from a few weeks to several months. It is mainly spread by the fecal-oral route, usually via contaminated food and water. Infected people can pass on the virus if they don't follow proper hygiene practices. Early symptoms include weakness, loss of appetite, nausea and fever, followed by the onset of jaundice.
Highly effective hepatitis A vaccines are available and should be considered by most travelers.
Vaccination should start 4 weeks before departure if possible. A booster dose is given 6 – 24 months later to provide protection for at least 10 years. Hepatitis A vaccination is recommended for all children starting at age 1 year, travelers to certain countries, and others at risk.
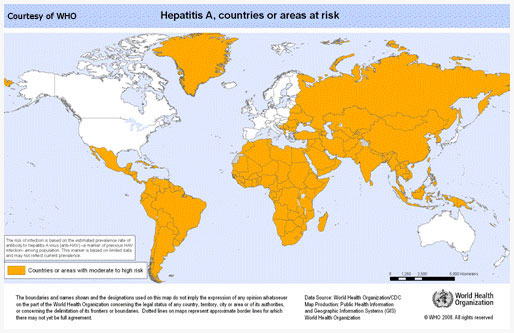
Hepatitis A is the most common vaccine preventable infection among travelers.
Link: CDC- Hepatitis A
Hepatitis B
Hepatitis B virus (HBV) is transmitted from person to person via infected blood and other body fluids. Important exposure includes unprotected sexual contact, transfusion of unscreened blood, exposure to unsterilized needles, body piercing, tattooing and contact with blood or open wounds. Hepatitis B is caused by one of the most common viruses worldwide.
Symptoms include flu-like complaints, loss of appetite, nausea, diarrhea, abdominal pains and jaundice. The liver infection may last from a few weeks to a serious long term (chronic) illness that can lead to liver disease or liver cancer. Hepatitis B vaccination is recommended for all infants, older children and adolescents who were not vaccinated previously, and adults at risk for HBV infection.
Three doses of vaccine constitute the complete series; the first two are usually given one month apart, with a third dose 6 months later.
A rapid schedule is day 0, day 7 and day 21. Recommended is a 4th dose after one year.
Immunization provides protection for at least 15 years.
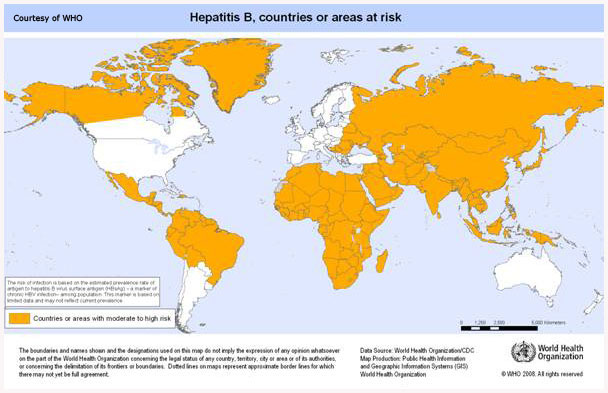
Link: CDC - Hepatitis B
Influenza
Influenza viruses evolve rapidly, changing their antigenic characteristics, so that vaccines need to be modified each year to be effective against currently circulating influenza strains. Influenza virus type A (H1N1 and H3N2) cause most of the widespread influenza epidemics. Transmission is by direct contact with droplets disseminated by unprotected cough and sneezing and contamination of hands.
Influenza is a seasonal disease occurring in winter; in the northern hemisphere from November to March and in the southern hemisphere from April to September. In tropical areas there is no clear seasonal pattern, and influenza may occur at any time of the year.
“Seasonal flu vaccination” is before the start of the influenza season.
WHO recommends a Flu shot to prevent influenza for persons with:- age > 65 years
- Diabetes Mellitus
- Chronic Pulmonary illness
- Cardio-vascular illness
- Renal dysfunction
- Immunosuppression due to medication, HIV etc.
- Contacts with high risk persons
Link: CDC - Influenza